Kernicterus
| Kernicterus | |
|---|---|
| Other names: Chronic bilirubin encephalopathy,[1] kernicterus spectrum disorder (KSD),[2] bilirubin induced neurological dysfunction (BIND)[2] | |
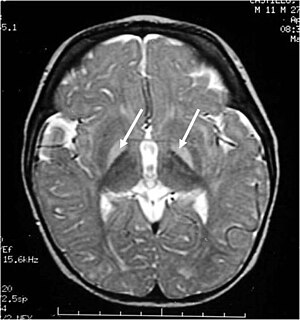 | |
| Brain MRI showing hyperintense basal ganglia lesions on T2-weighted images. | |
| Specialty | Pediatrics |
| Symptoms | Poor feeding, decreased activity, vomiting[1] |
| Complications | Seizures, cerebral palsy, hearing loss, vision problems, intellectual disability[3][1] |
| Causes | High levels of bilirubin[1] |
| Risk factors | Preterm, darker skin, bruising at birth, poor feeding[3] |
| Diagnostic method | Based on symptoms[1] |
| Differential diagnosis | Cerebral palsy, head trauma, TORCH infections, fetal alcohol syndrome, sepsis[4] |
| Prevention | Treatment of newborn jaundice[3] |
| Treatment | Symptomatic and supportive care[5] |
| Frequency | 0.2 to 2.7 per 100,000 newborns[6] |
Kernicterus is brain damage due to high levels of bilirubin in a baby's blood.[3] Early symptoms may include poor feeding, decreased activity, jaundice, and vomiting.[1][5] Complications may include seizures, cerebral palsy, hearing loss, vision problems, problems with teeth, and intellectual disability.[3][1]
Risk factors include preterm, darker skin, bruising at birth, Rh disease, poor feeding, and certain genetic conditions.[3][6][4] Other risks include low albumin, sepsis, and the use of certain medications like ceftriaxone and aspirin.[1] The underlying mechanism involves unbound bilirubin entering the central nervous system and resulting in toxicity to brain cells.[2] Diagnosis is suspected based on symptoms; however, can only be confirmed at autopsy.[1]
Prevention involves treating newborn jaundice with light therapy, increased milk intake, and sometimes exchange transfusion.[3] Once damage has occurred there is no specific treatment.[1] Measures at this point include symptomatic and supportive care.[5] Complications are often permanent, once they occur.[7] About 15% of newborn deaths in the developing world are the result of kernicterus.[4]
Kernicterus is relatively rare affecting about 0.2 to 2.7 per 100,000 newborns.[7][6] Males are more commonly affected than females.[6] In the United States Black babies are more commonly effected than white.[7] The condition was named in 1904 by Christian Georg Schmorl, though was described earlier in 1875 by Johannes Orth.[2]
Classification
Acute
Acute bilirubin encephalopathy (ABE) is an acute state of elevated bilirubin in the central nervous system. Clinically, it encompasses a wide range of symptoms. These include lethargy, decreased feeding, hypotonia or hypertonia, a high-pitched cry, spasmodic torticollis, opisthotonus, setting sun sign, fever, seizures, and even death. If the bilirubin is not rapidly reduced, ABE quickly progresses to chronic bilirubin encephalopathy. Technically it is not a form of kernicterus.
Chronic
Chronic bilirubin encephalopathy (CBE) is a chronic state of severe bilirubin-induced neurological lesions. Reduction of bilirubin in this state will not reverse the sequelae. Manifestations of CBE include:
- movement disorders – dyskinetic CP with often spasticity. 60% have severe motor disability (unable to walk).
- auditory dysfunction – auditory neuropathy (ANSD)
- visual/oculomotor impairments (nystagmus, strabismus, impaired upward or downward gaze, and/or cortical visual impairment). In rare cases, decreased visual acuity(blindness) can occur.
- dental enamel hypoplasia/dysplasia of the deciduous teeth,
- gastroesophageal reflux,
- impaired digestive function.
- slightly decreased intellectual function: Although most individuals (approximately 85%) with kernicterus fall in normal or dull-normal range.
- epilepsy is uncommon.
These impairments are associated with lesions in the basal ganglia, auditory nuclei of the brain stem, and oculomotor nuclei of the brain stem. Cortex and white matter are subtly involved. Cerebellum may be involved. Severe cortical involvement is uncommon.
Subtle
Subtle bilirubin encephalopathy (SBE) is a chronic state of mild bilirubin-induced neurological dysfunction (BIND). Clinically, this may result in neurological, learning and movement disorders, isolated hearing loss and auditory dysfunction.
- In the past it was thought that kernicterus (KI) often cause an intellectual disability. This was assumed due to difficulty with hearing, that is typically not detected in a normal audiogram accompanied by impairments of speech, with choreoathetosis. With advances in technology, this has proven to not be the case as those living with KI have repeatedly demonstrated their intelligence using Augmentative Communication devices[citation needed]. Although most individuals with kernicteric cerebral palsy have normal intelligence, some children with mild choreoathetosis develop dull normal intelligence or mild intellectual disability even without auditory dysfunction.
Causes
Unconjugated hyperbilirubinemia during the neonatal period describes the history of nearly all individuals who suffer from kernicterus. It is thought that the blood–brain barrier is not fully functional in neonates and therefore bilirubin is able to cross the barrier. Moreover, neonates have much higher levels of bilirubin in their blood due to:
- Although the severe hemolytic disease of the newborn is usually the cause of death, many children who barely survive the anemia exhibit permanent mental impairment or damage to motor areas of the brain because of precipitation of bilirubin in the neuronal cells, causing destruction of many, a condition called kernicterus. The rapid breakdown of fetal red blood cells immediately prior to birth (and subsequent replacement by normal adult human red blood cells). This breakdown of fetal red blood cells releases large amounts of bilirubin.[citation needed]
- Neonates cannot metabolize and eliminate bilirubin. The sole path for bilirubin elimination is through the uridine diphosphate glucuronosyltransferase isoform 1A1 (UGT1A1) proteins that perform a (SN2 conjugation) reaction called "glucuronidation". This reaction adds a large sugar to the bilirubin and makes it more water-soluble, so more readily excreted via the urine and/or the feces. The UGT1A1 enzymes are present, but not active until several months after birth in the newborn liver. Apparently, this is a developmental compromise since the maternal liver and placenta perform glucuronidation for the fetus. In the early 1980s a late-fetal change (30 – 40 weeks of gestation) in hepatic UGT1A1 (from 0.1% to 1.0% of adult activity levels) and post-natal changes that are related to birth age not gestational age were reported. Similar development of activities to pan-specific substrates were observed except for serotonin (1A4), where adult activities were observed in fetal (16 – 25 weeks) and neonatal liver up to 10 days old. More recently, individual UGT isoform development in infants and young children, including two fetal liver samples, were analyzed and showed that pediatric levels of mRNA and protein for UGT1A1 did not differ from adults, but activities were lower. Hence, the effects of UGT1A1 developmental delay in activation have been illuminated over the last 20–30 years. The molecular mechanism(s) for activating UGT1A1 remain unknown.[citation needed]
- Administration of aspirin to newborns. Aspirin displaces the bilirubin that was non-covalently attached to albumin in the blood stream, thus generating an increased level of free bilirubin which can cross the developing blood brain barrier. This can be life-threatening.[citation needed]
Bilirubin is known to accumulate in the gray matter of neurological tissue where it exerts direct neurotoxic effects. It appears that its neurotoxicity is due to mass-destruction of neurons by apoptosis and necrosis.
Risk factors
- Premature birth
- Rh incompatibility
- Polycythemia – often present in neonates
- Sulfonamides (e.g. co-trimoxazole) – displaces bilirubin from serum albumin
- Crigler–Najjar syndrome, type I
- G6PD deficiency
- Bruising
Gilbert's syndrome and G6PD deficiency occurring together especially increases the risk for kernicterus.[8]
Diagnosis
The diagnosis is based upon physical examination of moro reflex. Asymmetrical moro reflex indicate kernicterus[medical citation needed]. An xray also help to diagnose this condition. Asymmetrical moro reflex will indicate one sided brachial plexus injury. Neurological causes (including kernicterus) will have symmetric abnormal moro reflex ( or absent moro reflex).[citation needed]
Prevention
The only effective way at preventing kernicterus is to lower the serum bilirubin levels either by phototherapy or exchange transfusion. Visual inspection is never sufficient; therefore, it is best to use a bilimeter or blood test to determine a baby's risk for developing kernicterus. These numbers can then be plotted on the Bhutani nomogram.[citation needed]
Treatment
Currently no effective treatment exists for kernicterus. Future therapies may include neuroregeneration. A handful of patients have undergone deep brain stimulation, and experienced some benefit. Drugs such as baclofen, clonazepam, gabapentin, and artane are often used to manage movement disorders associated with kernicterus. Proton pump inhibitors are also used to help with reflux. Cochlear implants and hearing aids have also been known to improve the hearing loss that can come with kernicterus (auditory neuropathy – ANSD).[citation needed]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 "Kernicterus - Pediatrics". Merck Manuals Professional Edition. Archived from the original on 23 November 2021. Retrieved 21 March 2022.
- ↑ 2.0 2.1 2.2 2.3 Polin, Richard A.; Abman, Steven H.; Rowitch, David; Benitz, William E. (29 July 2021). Fetal and Neonatal Physiology E-Book. Elsevier Health Sciences. p. 1813. ISBN 978-0-323-71285-9. Archived from the original on 22 March 2022. Retrieved 21 March 2022.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 "What are Jaundice and Kernicterus? | CDC". Centers for Disease Control and Prevention. 11 December 2018. Archived from the original on 8 August 2016. Retrieved 23 February 2020.
- ↑ 4.0 4.1 4.2 Reddy, DK; Pandey, S (January 2022). "Kernicterus". PMID 32644546.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 5.0 5.1 5.2 Kock, Joanita De; Walt, Christa Van der (2004). Maternal and Newborn Care: A Complete Guide for Midwives and Other Health Professionals. Juta and Company Ltd. p. 31-66. ISBN 978-0-7021-6402-6. Archived from the original on 2022-03-22. Retrieved 2022-03-21.
- ↑ 6.0 6.1 6.2 6.3 Olusanya, BO; Kaplan, M; Hansen, TWR (August 2018). "Neonatal hyperbilirubinaemia: a global perspective". The Lancet. Child & adolescent health. 2 (8): 610–620. doi:10.1016/S2352-4642(18)30139-1. PMID 30119720.
- ↑ 7.0 7.1 7.2 Okolie, F; South-Paul, JE; Watchko, JF (1 December 2020). "Combating the Hidden Health Disparity of Kernicterus in Black Infants: A Review". JAMA pediatrics. 174 (12): 1199–1205. doi:10.1001/jamapediatrics.2020.1767. PMID 32628268.
- ↑ Cappellini MD, Di Montemuros FM, Sampietro M, Tavazzi D, Fiorelli G (1999). "The interaction between Gilbert's syndrome and G6PD deficiency influences bilirubin levels". British Journal of Haematology. 104 (4): 928–9. doi:10.1111/j.1365-2141.1999.1331a.x. PMID 10192462.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1 errors: missing periodical
- All articles with unsourced statements
- Articles with unsourced statements from July 2016
- Articles with invalid date parameter in template
- Articles with unsourced statements from December 2020
- Articles with unsourced statements from June 2019
- Neurological disorders
- Haemorrhagic and haematological disorders of fetus and newborn
- Cerebral palsy and other paralytic syndromes
- Neonatology
- Rare diseases
- RTT