Green nail syndrome
| Green nail syndrome | |
|---|---|
| Other names: Chloronychia | |
 | |
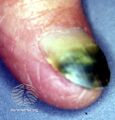
| Green nail syndrome-green coloration of the toe nail. | |
| Specialty | Dermatology |
| Symptoms | Green nails, inflammation of the surrounding skin, lifting of the nail at the tip[1] |
| Causes | Pseudomonas aeruginosa[2] |
| Risk factors | Occupations involving prolonged contact in water, other nail disorders[1] |
| Differential diagnosis | Onychomycosis, subungual hematoma, melanoma[1] |
| Treatment | Keep nails dry, Vinegar soaks, antibiotics[1] |
| Medication | 1% acetic acid solution (vinegar) twice daily[2] |
| Prognosis | May be resistant to treatment[1] |
Green nail syndrome, also known as Goldman–Fox Syndrome, is characterised by green discolouration of nails, associated with inflammation of the surrounding skin and lifting of the nail at the tip.[1] It generally affects one or two nails.[1]
The condition is due to pyoverdin and pyocyanin producing Pseudomonas aeruginosa that can develop in individuals whose hands are frequently submerged in water.[2][3] It may occur as transverse green stripes that are ascribed to intermittent episodes of infection.[4] There may be other nail disorders such as psoriasis or paronychia.[1] Risk factors include certain having a pre-existing fungal infection of the nail and certain occupations such as hairdressers and healthcare workers.[1] Onychomycosis, subungual hematoma, and melanoma may appear similar.[1] Exposure to copper in water may also result in green nails.[4]
Treatment generally involves keeping the nails dry, and soaking the affected fingers in 1% acetic acid solution (vinegar) twice daily.[1][2] Fluoroquinolone antibiotics such as ciprofloxacin or levofloxacin by mouth are other options.[1] An alternative treatment is applying neosporin solution twice daily after trimming the nail.[2] Removing the affected is sometimes required.[1]
Symptoms and signs
The most common symptom of Green Nail Syndrome is the discolouration of the infected nail as it turns a dark green colour, due to the bacteria secreting the green pigments Pyoverdin and Pyocyanin.[5][6][7][8] The patient can also suffer from tenderness surrounding the infected nail along with redness and swelling.[5]
-
Green nail due to pseudomonas infection
-
Green nail due to pseudomonas infection
-
Green foot
-
Pseudomonas-candida infection
Causes
It is most commonly caused by the bacteria “Pseudomonas Aeruginosa”,[5][6][8][9] which thrives in moist conditions.[6] Green Nail Syndrome is linked to regular submergence of one’s hands in water, detergents and soils.[10]
Green Nail Syndrome is caused by exposing the nail to the bacterial organism, which leads to opportunistic infection.[6] These bacteria are typically found in water sources and soil. They grow and multiply rapidly in moist environments such as sinks, swimming pools and sponges.[5]
The seal between the nail and finger acts as a physical barrier to prevent this kind of infection, however hyper-hydration or destruction of the epidermis can impair the barrier, allowing the colonisation of the bacteria.[6]
It is possible for a patient to transfer Green Nail Syndrome from an infected nail to a non-infected nail via self-inoculation, in transferring the bacteria to a new infection site.[6]
Predispositions
Those working in jobs requiring them to have their hands submerged in water or soil for prolonged periods of time on a regular basis.[6][8] These include housewives, dishwashers, bakers, barbers, medical personnel[8] and farmers. Patients in hospital for non-related issues have contracted the infection, indicating that Green Nail Syndrome can be a hospital acquired infection.[6]
The elderly and people who have suffered trauma to a finger or nail are predisposed to contracting Green Nail Syndrome.[10] Patients who are already suffering with nail diseases such as onycholysis and onychotillomania[11] are at higher risk of contracting Green Nail Syndrome.
Predisposition to Green Nail Syndrome has also been linked to manicures, heat, dermatitis, ulcerations. Occlusions and excess sweating.[6] Higher risk of contracting the infection is also linked to soccer players and military personnel due to the prolonged periods of time in which they exercise while wear tight fitting shoes[5] as well as immunosuppressed persons and those with weakened epidermis barrier.
Bacteria

Pseudomonas Aeruginosa[6][8] species of bacteria are the most common causes of Green Nail Syndrome. Nail scrapings have identified Aspergillus,[6] Candida[6][8] and Klebsiella Pneumoniae[11] species present at the infected nail site. It is unsure whether these are causative organisms or simply coinfections alongside Pseudomonas Aeruginosa.[6]
Diagnosis
Diagnosis can typically be made from a physical examination of the nail. If necessary, a gram stain[6] or bacteriological culture of nail scrapings[6][9] can be performed in order to identify the presence of bacteria.
There are shortcomings however in conducting a culture because the infection can be present a distance from the nail site, and as a result return a false negative result.[6] A sample of infected nail can be submerged in distilled water to perform a pigment solubility test, within 24 hours the liquid will turn blue green in colour indicating the presence of Pseudomonas Aeruginosa.[6]
Differential diagnosis
Green Nail Syndrome can be misdiagnosed with Aspergillus infections, Malignant melanoma, Subungual hematomas.[8] The use of green dye, paint or chemical lacquers can also lead to confusion.[8]
Prevention
Preventative measures should be implemented by those who are most at risk of contracting Green Nail Syndrome due to their predisposition or lifestyle and workplace choices. Wearing waterproof gloves or gum boots can be effective in preventing prolonged exposure of the nails to water.[6] Avoiding trauma that could lead to the destruction of the epidermis seal is on the nails is a priority in preventing green nail syndrome recurrences.[6]
Treatment
Treatment for Green Nail Syndrome varies greatly depending on the severity of the infection and the length of time it has been present. There are many medically approved options when a patient is treated by a medical professional. For persons who are unable to seek medical help there are also alternative treatments that have been trialled successfully.[6]
Medical Treatment
There are several medical treatment options, depending on the severity of the infection and how long it has been present. The least invasive treatment includes soaking the nail in alcohol and regularly trimming the nail back,[8] to dry out the area and prevent bacterial colonisation.[9] Moderate cases of Green Nail Syndrome are prescribed topical antibiotics (silver sulfadiazine, gentamicin, ciprofloxacin, bacitracin and polymyxin B)[9] or oral antibiotics (ciprofloxacin),[5][12][11][9] antiseptic creams,[12] tobramycin eye drops have also been reported to be effective. In severe cases, surgical removal of the infected nail may be required.[12][5][9] The patient should always avoid further trauma to the infected nail regardless of the stage of treatment they received.[5]
Alternative Treatment
Some at-home treatments have been successfully trialled in treating mild cases of Green Nail Syndrome. Soaking the nails in vinegar or a chlorine bleach solution (diluted with water 1:4) at regular intervals can be used when medical help is not accessible to the patient.[5]
Patient management and recovery
In mild to moderate cases, where the infection clears with minimal medical intervention, the patient should ensure the nail is kept clean and dry and avoid hyper-hydration. Humid climates could lead to a longer recovery than dry climes due to inability to expose the site to very dry air.[6] In cases where surgery is necessary, patients should follow their medical professional’s post-surgery advice.
Cases
- Green nail syndrome in nail salons -Pseudomonas can be transferred among clients in a nail salon if appropriate hygiene standards are not up kept. While the bacteria wouldn’t typically survive on the nail shaping equipment, unclean conditions could allow for it to transfer from equipment to client’s nails repeatedly.[13] When technicians are presented with a client that has suspected green nail syndrome, they shouldn’t continue the normal treatment of painting nails, applying acrylic nails or otherwise. This is due to the application of liquids and oils creating an environment which the bacteria be trapped and treatment will not be possible without the removal of these polishes.[13] As chief science advisor at CND Doug Schoon states “it creates a nearly oxygen free environment, which these bacteria just love”. Nail technicians are not qualified to treat green nail syndrome and should educate the client[14] on the condition and encourage them to seek medical treatment before returning to the nail salon.[13]
- Green nail syndrome and working with chemicals -A man working with in a job where he was regularly mixing chemicals developed green nail syndrome.[15] While he mostly wore latex gloves, he reported they would become moist and often he would remove them to clean his hands and utensils.[16] The combination of moisture within his gloves and contact with chemicals caused his nails to lift from the nail bed. He developed severe green nail syndrome and was treated with topical antibiotics, which cleared up the infection within 6 months.[16] It was noted that latex gloves were not suitable for his line of work and more robust rubber gloves should be used.[15]
- Green nail syndrome and Basel Cell Carcinomas -There have been cases where a Basel Cell Carcinoma has been present in conjunction with Green Nail Syndrome.[6] Carcinomas are not common in the area surrounding the nail bed.[17] However, if a Carcinoma is suspected in conjunction with or in place of green nail syndrome, a biopsy should be conducted immediately.[17] The Indian Journal of Dermatology states "Early diagnosis can enable the physician to render simpler nondestructive modalities of treatment. In this article, we describe such a case of longstanding BCC of this region mimicking a traumatic ulcer".[17]
- Green nail syndrome transfer within hospitals -Medical professionals with Green Nail Syndrome have been reported to have transferred the infection to patients in hospitals.[6] Five surgical site infections during 2001 were linked to a cardiac surgeon with the infection who didn't routinely use double gloves.[18] The surgeon's infected nail was surgically removed and no further transfers of the infection were reported.[18]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Heymann, Warren R. (3 February 2021). "Going green: The complexities of the green nail syndrome". www.aad.org. Archived from the original on 20 March 2023. Retrieved 31 May 2023.
- ↑ 2.0 2.1 2.2 2.3 2.4 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "14. Bacterial infections". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 270. ISBN 978-0-323-54753-6. Archived from the original on 2023-06-30. Retrieved 2023-06-01.
- ↑ "Pseudomonas aeruginosa Infections: Clinical Presentation". eMedicine. Archived from the original on 2 February 2014. Retrieved 1 February 2014.
- ↑ 4.0 4.1 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "33. Diseases of the skin appendages". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 790. ISBN 978-0-323-54753-6. Archived from the original on 2023-06-30. Retrieved 2023-05-31.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 American Osteopathic College of Dermatology. (2019). Green Nail Syndrome. Available at: https://cdn.ymaws.com/www.aocd.org/resource/resmgr/patientresources/1/GREEN_NAIL_SYNDROME.pdf
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 6.20 6.21 6.22 "Green Nail Syndrome (GNS, Pseudomonas nail infection, chloronychia, green striped nails, chromonychia)". Dermatology Advisor. 2019-03-13. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ "You have been blocked". www.patientcareonline.com. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Clark, K., & Davison, L. (2006). Green Nail Syndrome. NJ, USA: MJH Healthcare holdings LLC. Available at: https://www.patientcareonline.com/infection/green-nail-syndrome
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Matsuura, H.; Senoo, A.; Saito, M.; Hamanaka, Y. (2017-09-01). "Green nail syndrome". QJM: An International Journal of Medicine. 110 (9): 609. doi:10.1093/qjmed/hcx114. ISSN 1460-2725. PMID 28911027. Archived from the original on 2020-06-03. Retrieved 2021-10-10.
- ↑ 10.0 10.1 Chiriac, Anca; Brzezinski, Piotr; Foia, Liliana; Marincu, Iosif (2015-01-14). "Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons". Clinical Interventions in Aging. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ 11.0 11.1 11.2 Hengge, U. R.; Bardeli, V. (2009). "Green Nails | NEJM". New England Journal of Medicine. 360 (11): 1125. doi:10.1056/nejmicm0706497. PMID 19279344. Archived from the original on 2022-04-07. Retrieved 2020-06-03.
- ↑ 12.0 12.1 12.2 "Green Nail Syndrome - Skin Disorders". MSD Manual Consumer Version. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ 13.0 13.1 13.2 "What Is Pseudomonas?". www.nailsmag.com. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ Schoon, Doug (2016). Face-To-Face with Doug Schoon Volume I: Science and Facts about Nails/nail Products for the Educationally Inclined. Schoon Scientific. ISBN 978-0997918601.
- ↑ 15.0 15.1 Leung, Lawrence K.; Harding, John (2015-06-03). "A chemical mixer with dark-green nails". BMJ Case Reports. 2015: bcr2014209203. doi:10.1136/bcr-2014-209203. ISSN 1757-790X. PMC 4460363. PMID 26040827.
- ↑ 16.0 16.1 "A case of green nail syndrome". myDr.com.au. 2016-04-13. Archived from the original on 2020-06-03. Retrieved 2020-06-03.
- ↑ 17.0 17.1 17.2 Bandyopadhyay, Debabrata; Sen, Sumit (2011). "Periungual basal cell carcinoma: A case report with review of literature". Indian Journal of Dermatology. 56 (2): 220–222. doi:10.4103/0019-5154.80425. ISSN 0019-5154. PMC 3108529. PMID 21716555.
- ↑ 18.0 18.1 La, Mermel; M, McKay; J, Dempsey; S, Parenteau (October 2003). "Pseudomonas Surgical-Site Infections Linked to a Healthcare Worker With Onychomycosis". Infection Control and Hospital Epidemiology. 24 (10): 749–52. doi:10.1086/502125. PMID 14587936. Archived from the original on 2020-06-03. Retrieved 2020-06-03.