Cyclosporiasis
| Cyclosporiasis | |
|---|---|
| Other names: cyclosporosis | |
 | |
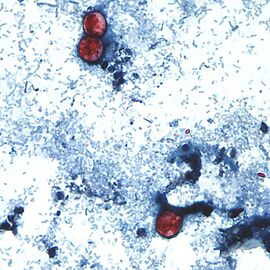
| Cyclospora cayetanensis | |
| Specialty | Infectious disease |
| Symptoms | Watery diarrhea, cramping, nausea |
| Causes | Cyclospora cayetanensis |
| Diagnostic method | PCR tests |
| Treatment | Trimethoprim/sulfamethoxazole |
Cyclosporiasis is a disease caused by infection with Cyclospora cayetanensis, a pathogenic protozoan transmitted by feces or feces-contaminated food and water.[1] Cyclosporiasis was virtually unknown in developed countries until awareness increased due to several outbreaks linked with fecally contaminated imported produce. C. cayetanensis has since emerged as an endemic cause of diarrheal disease in tropical countries and food-borne infections in developed nations.[2]
It is not spread from person to person, but can be a hazard for travelers or tourists as a cause of traveler's diarrhea.[3][4][5]
Signs and symptoms
The clinical presentation of Cyclosporiasis is as follows, C. cayetanensis causes gastroenteritis, with the extent of the illness varying based on age, condition of the host, and size of the infectious dose. [6]
Symptoms include "watery diarrhea, loss of appetite, weight loss, abdominal bloating and cramping, nausea, fatigue, and fever", though this can be augmented in more severe cases by vomiting, weight loss, and diarrhea. [6][5][7]
Cause
Cyclosporiasis primarily affects humans and other primates. When an oocyst of Cyclospora cayetanensis enters the small intestine, it invades the mucosa, where it incubates for about one week. After incubation, the infected person begins to experience severe watery diarrhea, bloating, fever, stomach cramps, and muscle aches.[8][9]
The parasite particularly affects the jejunum of the small intestine. Of nine patients in Nepal who were diagnosed with cyclosporiasis, all had inflammation of the lamina propria along with an increase of plasma in the lamina propria. Oocysts were also observed in duodenal aspirates.[10]
Persons living or traveling in developing tropical or subtropical areas may be at an increased risk of acquiring C. cayetanensis, as it is endemic in these areas. Infections in endemic regions tend to show a marked seasonality that is poorly understood, whereas North American outbreaks occur most frequently in summer.[11][2][12]
Consuming food or water while visiting developing countries is a well-documented way of developing traveler's diarrhea. Travelers are often warned against such actions, but over 70 percent of certain produce items consumed in the United States are imported from developing countries, making "traveler's diarrhea" possible without international travel.[13]
Diagnosis
Methods have been established for positive diagnosis of the protozoan: microscopic detection in stool samples of oocysts, recovering oocysts in intestinal fluid/small bowel biopsy specimens, demonstration of oocyst sporulation, and amplification by polymerase chain reaction of C. cayetanensis DNA. One negative result should not discount the possibility of C. cayetanensis, tests involving fresh stool samples over the next few days should also be considered.[14][15][7]
Diagnosis can be difficult due to the lack of recognizable oocysts in the feces. PCR-based DNA tests and acid-fast staining can help with identification.[14][7]
-
a,b)Unsporulated oocyst of Cyclospora cayetanensis in an unstained stool preparation
-
a-c)Cyclospora cayetanensis oocysts under microscopy
Prevention
No vaccine against this pathogen is available.[16] Since infection occurs via fecally contaminated food and water in endemic environments, several simple solutions have been suggested for the prevention of C. cayetanensis infections. The simplest is to warn travelers not to visit regions where the protozoan is endemic, especially when the season is best for spreading. Travelers also should be aware that treatment of water or food with chlorine or iodine is unlikely to kill Cyclospora oocysts.[17] Additionally, better health practices in the originating agricultural setting—such as making sure produce watering systems are not pulling water that has access to human feces; using filtering systems such as a 1 micron absolute carbon filtration system will reduce the presence of Cyclospora, drastically decreasing the incidence of the spread of this parasite.[2]
Treatment

Most people who have healthy immune systems will recover without treatment, however, the illness may last for a few days to a month or longer. Symptoms may seem to go away and then return one or more times (relapse). Antidiarrheal medicine may help reduce diarrhea, people who are in poor health or who have weakened immune systems may be at higher risk for severe or prolonged illness.[18]
The infection is often treated with trimethoprim/sulfamethoxazole, also known as Bactrim or co-trimoxazole, because traditional anti-protozoal drugs are not sufficient.[19]
Epidemiology
Outbreaks
Although it was initially thought that Cyclospora was confined to tropical and subtropical regions, occurrences of cyclosporiasis are becoming more frequent in North America. According to the Centers for Disease Control and Prevention, there have been 11 documented cyclosporiasis outbreaks in the U.S. and Canada since the 1990s. The CDC also recorded 1,110 laboratory-confirmed sporadic instances of cyclosporiasis.[20]
Between June and August 2013, multiple independent outbreaks of the disease in the U.S. sickened at least 631 people across 25 states.[21][22] Investigations later identified a bagged salad mixture as the cause of an outbreak in Iowa and Nebraska.[23]
In 2015, the CDC was notified of 546 persons with confirmed cyclosporiasis infection across 31 states. Cluster investigations in Texas, where the greatest number of infections was reported, indicated that contaminated cilantro was the culprit.[24] During July 21–August 8, 2017, the Texas Department of State Health Services (DSHS) was notified of 20 cases of cyclosporiasis among persons who dined at a Mediterranean-style restaurant chain (chain A) in the Houston area.[25]On July 31, 2018, the United States Department of Agriculture (USDA) issued a public health alert for certain beef, pork and poultry salad and wrap products potentially contaminated with Cyclospora,[26] the contamination came from the chopped romaine lettuce used in these products.
In June 2020, the CDC and other regulatory bodies began investigating an outbreak of Cyclosporiasis in the Midwestern United States linked to bagged salad mix.[27] On June 27, 2020, Fresh Express announced a voluntary recall of over 91 Fresh Express and private label salad products.[28]
Summary of U.S. foodborne outbreaks of cyclosporiasis, 2000–2014 [29]


| Year(s)* | Month(s)* | Jurisdiction(s)* | No. of cases† | Food vehicle and source, if identified‡ |
|---|---|---|---|---|
| 2000 | May | Georgia | 19 | Raspberries and/or blackberries (suspected) |
| 2000 | June | Pennsylvania | 54 | Raspberries |
| 2001 | January–February | Florida | 39 | |
| 2001 | January | New York City | 3 | |
| 2001–02 | December–January | Vermont | 22 | Raspberries (likely) |
| 2002 | April–May | Massachusetts | 8 | |
| 2002 | June | New York | 14 | |
| 2004 | February | Texas | 38 | |
| 2004 | February | Illinois | 57 | Basil (likely) |
| 2004 | May | Tennessee | 12 | |
| 2004 | May–June | Pennsylvania | 96 | Snow peas from Guatemala |
| 2005 | March–May | Florida | 582 ¶ | Basil from Peru |
| 2005 | May | South Carolina | 6 | |
| 2005 | April | Massachusetts | 58 | |
| 2005 | May | Massachusetts | 16 | |
| 2005 | June | Connecticut | 30 | Basil (suspected) |
| 2006 | June | Minnesota | 14 | |
| 2006 | June | New York | 20 | |
| 2006 | July | Georgia | 3 | |
| 2008 | March | Wisconsin | 4 | Sugar snap peas (likely) |
| 2008 | July | California | 45 ¶ | Raspberries and/or blackberries (likely) |
| 2009 | June | District of Columbia | 34 | |
| 2011 | June | Florida | 12 | |
| 2011 | July | Georgia | 100 | |
| 2012 | June–July | Texas | 16 | |
| 2013** | June | Iowa and Nebraska | 161 | Bagged salad mix from Mexico |
| 2013** | June–July | Texas | 38 | Cilantro from Mexico |
| 2013 | July | Wisconsin | 8 | Berry salad (suspected) |
| 2014 | June | Michigan | 14 | |
| 2014†† | June–July | Texas | 26 | Cilantro from Mexico |
| 2014 | July | South Carolina | 13 |
(*)The entries in the first three columns refer to the known or likely year(s), month(s), and jurisdiction(s) in which the exposure(s) to Cyclospora occurred.
(**)For the purposes of this table, the exposure month(s) and case counts are limited to those explicitly linked in the investigations to the food item specified in the last column.
† The case counts include laboratory-confirmed and probable cases of cyclosporiasis. By definition, each outbreak included at least two linked cases, at least one of which was laboratory confirmed.
‡ A food vehicle is specified only if a single ingredient or commodity was identified in an outbreak investigation.
¶ Cases that occurred in Canadian travelers to the United States were not included.
†† For the purposes of this table, the exposure months and the case count for the outbreak in Texas are limited to those explicitly linked in the investigations to the food item specified in the last column
History
The first recorded cases of cyclosporiasis in humans were as recent as 1977, 1978, and 1979. They were reported by Ashford, a British parasitologist who discovered three cases while working in Papua New Guinea. Ashford found that the parasite had very late sporulation, from 8–11 days, making the illness difficult to diagnose. When examining feces, the unsporulated oocysts can easily be mistaken for fungal spores, and thus can be easily overlooked.[31]
In 2007, Indian researchers published a case report that found an association between Cyclospora infection and Bell's palsy. This was the first reported case of Bell’s palsy following chronic Cyclospora infection.[32] In addition to other extra-intestinal reports, cyclosporiasis might be involved in either reversible neuronal damage or other unknown mechanisms that lead to Guillain-Barré syndrome[15]
In 2010, a report of Cyclospora transmission via swimming in the Kathmandu Valley was published in the Journal of Institute of Medicine.[33] The researchers found that openly defecated human stool samples around the swimmer's living quarters and near the swimming pool were positive for Cyclospora. However, they did not find the parasite in dog stool, bird stool, cattle dung, vegetable samples, or water samples. They concluded that pool water contaminated via environmental pollution might have caused the infection, as the parasite can resist chlorination in water.[34]
Cyclosporiasis infections have been well reported in Nepal. In one study, Tirth Raj Ghimire, Purna Nath Mishra, and Jeevan Bahadur Sherchan collected samples of vegetables, sewage, and water from ponds, rivers, wells, and municipal taps in the Kathmandu Valley from 2002 to 2004.[35] They found Cyclospora in radish, cauliflower, cabbage, and mustard leaves, as well as sewage and river water. This first epidemiological study determined the seasonal character of cyclosporiasis outbreaks in Nepal during the rainy season, from May to September.[36]
Cyclosporiasis and AIDS

The beginning of the AIDS epidemic in the early 1980s, cyclosporiasis was identified as one of the most important opportunistic infections among AIDS patients.[2]In 2005, Ghimire and Mishra reported a case of cyclosporiasis in a patient with low hemoglobin and suggested that this coccidian might be involved in reducing hemoglobin due to lack of immune system.[37]
In 2006, their groups published a paper about the role of cyclosporiasis in HIV/AIDS patients and non-HIV/AIDS patients in the Kathmandu Valley.[38]In 2008, Indian researchers published a report about the epidemiology of Cyclospora in HIV/AIDS patients in Kathmandu.[39] They examined samples of soil, river water, sewage, chicken stool, dog stool, and stool in the streets, and found them positive for Cyclospora. They also evaluated several risk factors for cyclosporiasis in AIDS patients.[39]
When infected with cyclospora, AIDS individuals tend to have greater weight loss than non-AIDS individuals due to diarrhea[40]
References
- ↑ Talaro, Kathleen P., and Arthur Talaro. Foundations in Microbiology: Basic Principles. Dubuque, Iowa: McGraw-Hill, 2002.
- ↑ 2.0 2.1 2.2 2.3 Ortega, Ynés R.; Sanchez, Roxana (January 2010). "Update on Cyclospora cayetanensis , a Food-Borne and Waterborne Parasite". Clinical Microbiology Reviews. 23 (1): 218–234. doi:10.1128/CMR.00026-09. ISSN 0893-8512. Archived from the original on 8 December 2022. Retrieved 18 December 2022.
- ↑ "Cyclosporiasis - About the Disease - Genetic and Rare Diseases Information Center". rarediseases.info.nih.gov. Archived from the original on 12 May 2021. Retrieved 15 December 2022.
- ↑ Giangaspero, Annunziata; Gasser, Robin B. (July 2019). "Human cyclosporiasis". The Lancet. Infectious Diseases. 19 (7): e226–e236. doi:10.1016/S1473-3099(18)30789-8. ISSN 1474-4457. Archived from the original on 12 December 2022. Retrieved 15 December 2022.
- ↑ 5.0 5.1 Nutrition, Center for Food Safety and Applied (17 November 2022). "Cyclosporiasis and Fresh Produce". FDA. Archived from the original on 30 November 2022. Retrieved 16 December 2022.
- ↑ 6.0 6.1 Prevention, CDC-Centers for Disease Control and (12 April 2019). "CDC - Cyclosporiasis - Disease". www.cdc.gov. Archived from the original on 9 July 2022. Retrieved 3 November 2022.
- ↑ 7.0 7.1 7.2 "Cyclosporiasis - Chapter 4 - 2020 Yellow Book | Travelers' Health | CDC". wwwnc.cdc.gov. Archived from the original on 17 December 2022. Retrieved 17 December 2022.
- ↑ Prevention, CDC-Centers for Disease Control and (12 April 2019). "CDC - Cyclosporiasis - Biology". www.cdc.gov. Archived from the original on 8 December 2022. Retrieved 12 December 2022.
- ↑ Karanja, RM; Gatei, W; Wamae, N (June 2007). "Cyclosporiasis: an emerging public health concern around the world and in Africa". African health sciences. 7 (2): 62–7. PMID 17594281. Archived from the original on 14 June 2020. Retrieved 21 December 2022.
- ↑ Sanchez, Roxana; Ortega, Ynés R. (2005-10-26). "Update on Cyclospora cayetanensis, a Food-Borne and Waterborne Parasite | Clinical Microbiology Reviews". Clinical Microbiology Reviews. Cmr.asm.org. 23 (1): 218–234. doi:10.1128/CMR.00026-09. PMC 2806662. PMID 20065331.
- ↑ Prevention, CDC-Centers for Disease Control and (17 September 2020). "CDC - Cyclosporiasis - General Information - Cyclosporiasis FAQs". www.cdc.gov. Archived from the original on 14 December 2022. Retrieved 13 December 2022.
- ↑ Casillas, Shannon M. (2019). "Cyclosporiasis Surveillance — United States, 2011–2015". MMWR. Surveillance Summaries. doi:10.15585/mmwr.ss6803a1. Archived from the original on 8 December 2022. Retrieved 23 December 2022.
- ↑ NaTashua Davis, ed. (Fall 2002). "The McNair Journal" (PDF). University of Missouri-Columbia. Archived from the original (PDF) on 2020-09-26. Retrieved 2022-12-08.
- ↑ 14.0 14.1 Shlim, David R. (December 2002). "Cyclospora cayetanesis". Clinics in Laboratory Medicine. 22 (4): 927–936. doi:10.1016/s0272-2712(02)00025-2. ISSN 0272-2712. Archived from the original on 9 December 2022. Retrieved 9 December 2022.
- ↑ 15.0 15.1 Li, Junqiang; Cui, Zhaohui; Qi, Meng; Zhang, Longxian (2020). "Advances in Cyclosporiasis Diagnosis and Therapeutic Intervention". Frontiers in Cellular and Infection Microbiology. 10: 43. doi:10.3389/fcimb.2020.00043. ISSN 2235-2988. Archived from the original on 9 December 2022. Retrieved 19 December 2022.
- ↑ "Cyclosporiasis - Prevention & Control". CDC - Centers for Disease Control and Prevention. 2018-06-15. Archived from the original on 2022-11-29. Retrieved 2022-12-18.
- ↑ "CDC - Cyclosporiasis - Epidemiology & Risk Factors". CDC - Centers for Disease Control and Prevention. 2018-05-10. Archived from the original on 2022-12-14. Retrieved 2022-12-18.
- ↑ Prevention, CDC - Centers for Disease Control and (2018-10-18). "CDC - Cyclosporiasis - Treatment". Archived from the original on 2022-12-08. Retrieved 2022-12-08.
- ↑ "Cyclosporiasis - Infectious Diseases". MSD Manual Professional Edition. Archived from the original on 14 December 2022. Retrieved 13 December 2022.
- ↑ "Surveillance for Laboratory-Confirmed Sporadic Cases of Cyclosporiasis --- United States, 1997--2008". cdc.gov. Archived from the original on 2022-06-17. Retrieved 2022-08-12.
- ↑ "Case Count Maps - Outbreak Investigations 2013 - Cyclosporiasis - CDC". cdc.gov. 2019-04-12. Archived from the original on 2022-04-12. Retrieved 2022-08-12.
- ↑ "CDC: 425 cases of cyclospora infection identified across 16 states". cbsnews.com. 5 August 2013. Archived from the original on 16 August 2013. Retrieved 12 August 2022.
- ↑ http://www.idph.state.ia.us/IDPHChannelsService/file.ashx?file=2721EA4A-DB6B-4746-9FF4-0BF09C9BF3BE Archived 2016-03-04 at the Wayback Machine Iowa Cyclospora Outbreak 2013 /Outbreak Update 7.31.13, Iowa State Department of Public Health. Downloaded 6 Aug 2013.
- ↑ "Outbreak Investigations 2015 | Cyclosporiasis | CDC". Cdc.gov. 2019-04-12. Archived from the original on 2019-06-15. Retrieved 2019-08-21.
- ↑ Keaton, A. A.; Hall, N. B.; Chancey, R. J.; Heines, V.; Cantu, V.; Vakil, V.; Long, S.; Short, K.; Franciscus, E.; Wahab, N.; Haynie, A.; Gieraltowski, L.; Straily, A. (2018-06-01). "Notes from the Field: Cyclosporiasis Cases Associated with Dining at a Mediterranean-Style Restaurant Chain — Texas, 2017 | MMWR". MMWR. Morbidity and Mortality Weekly Report. Cdc.gov. 67 (21): 609–610. doi:10.15585/mmwr.mm6721a5. PMC 6038903. PMID 29851947.
- ↑ "FSIS Issues Public Health Alert for Beef, Pork and Poultry Salad and Wrap Products due to Concerns about Contamination with Cyclospora". usda.gov. 31 July 2018. Archived from the original on 19 January 2021. Retrieved 12 August 2022.
- ↑ "Cyclosporiasis Outbreak Investigations — United States, 2020". www.cdc.gov. 2020-06-26. Archived from the original on 2020-06-26. Retrieved 2020-06-27.
- ↑ "Update: New Bagged Salad Products Linked to Cyclospora Outbreak". 30 June 2020. Archived from the original on 23 June 2021. Retrieved 12 August 2022.
- ↑ "U.S. Foodborne Outbreaks of Cyclosporiasis—2000–2014". Centers for Disease Control and Prevention. Archived from the original on 7 July 2015. Retrieved 30 June 2015.
- ↑ Hassan, Greg Botelho,Carma (31 July 2013). "Salad mix blamed for cyclospora outbreak in Nebraska, Iowa". CNN. Retrieved 20 December 2022.
- ↑ Strausbaugh, Larry (1 October 2000). "Cyclospora cayetanensis: A Review, Focusing on the Outbreaks of Cyclosporiasis in the 1990s". Clinical Infectious Diseases. 31 (4): 1040–1057. doi:10.1086/314051. PMID 11049789.
- ↑ Ghimire TR, Mishra PN, Sherchand JB, Ghimire LV: Bell’s Palsy and Cyclosporiasis: Causal or Coincidence? Nepal Journal of Neuroscience 4:86- 88, 2007. http://neuroscience.org.np/neuro/issues/uploads/abstract_K3M0aH6IUP.pdf Archived 2018-07-08 at the Wayback Machine
- ↑ T. R. Ghimire, L.V. Ghimire, R.K. Shahu, P.N. Mishra (April 2010). "Cryptosporidium and Cyclospora infection transmission by swimming". Journal of Institute of Medicine. 32 (1). doi:10.3126/jiom.v32i1.4003. Archived from the original on 2017-09-22. Retrieved 2019-08-21.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Ghimire TR, Ghimire LV, Shahu RK, Mishra PN. Cryptosporidium and Cyclospora infection transmission by swimming. Journal of Institute of Medicine. 2010; 32 (1): 43–45.https://www.nepjol.info/index.php/JIOM/article/download/4003/3392 Archived 2017-09-22 at the Wayback Machine
- ↑ Ghimire TR, Mishra PN, Sherchand JB. The seasonal outbreaks of Cyclospora and Cryptosporidium in Kathmandu, Nepal. Journal of Nepal Health Research Council. 2005; 3(1): 39–48.http://jnhrc.com.np/index.php/jnhrc/article/view/99/96
- ↑ Ghimire TR, Mishra PN, Sherchand JB. The seasonal outbreaks of Cyclospora and Cryptosporidium in Kathmandu, Nepal. Journal of Nepal Health Research Council. 2005; 3(1): 39–48. http://jnhrc.com.np/index.php/jnhrc/article/view/99/96 Archived 2020-12-01 at the Wayback Machine
- ↑ Ghimire TR, Mishra PN. Intestinal parasites and Haemoglobin concentration in the people of two different areas of Nepal. Journal of Nepal Health Research Council. 2005; 3(2): 1–7.http://jnhrc.com.np/index.php/jnhrc/article/view/103/100
- ↑ Ghimire TR, Mishra PN. Intestinal parasites in the Human Immunodeficiency Virus Infected Patients in Kathmandu, Nepal. The Nepalese Journal of Zoology. 2006; 1(1): 9–19.
- ↑ 39.0 39.1 Ghimire TR, Mishra PN, Sherchan JB. Epidemiology of Cyclospora cayetanensis and other intestinal parasites in the HIV infected patients in Kathmandu, Nepal. Journal of Nepal Health Research Council. 2008; 6(12): 28–37.https://www.nepjol.info/index.php/JNHRC/article/download/2441/2177
- ↑ Zhang, Long; Wang, Rong-Jun; Zhao, Guang-Hui; Li, Jun-Qiang (21 April 2021). Cyclospora and Cyclosporiasis: Epidemiology, Diagnosis, Detection, and Control. Academic Press. p. 49. ISBN 978-0-12-821622-4.
External links
| Classification | |
|---|---|
| External resources |
- Cyclosporiasis Archived 2013-08-05 at the Wayback Machine at Centers for Disease Control & Prevention
- Cyclospora Infection at MayoClinic.com

