Eumycetoma
| Mycetoma | |
|---|---|
| Other names: Madura foot | |
 | |
| Madura Foot[1] | |
| Specialty | Infectious diseases[2] |
| Symptoms | Painless wet nodule, ulceration, swelling, bone deformity, grainy discharge[3] |
| Causes | Madurella mycetomatis, Madurella grisea, Leptosphaeria senegalensis, Curvularia lunata, Scedosporium apiospermum, Neotestudina rosatii, Acremonium spp. and Fusarium spp.[2] |
| Diagnostic method | Microscopy, biopsy, and culture,[4] medical imaging, ELISA, immunodiffusion, PCR with DNA sequencing[5] |
| Differential diagnosis | Actinomycetic mycetoma[3] |
| Treatment | Surgery, antifungal medicines[3] |
| Medication | Itraconazole, posaconazole, voriconazole[5] |
| Prognosis | Recurrence is common[6] |
| Frequency | Endemic in Africa, India and South America[3] M>F[5] |
Eumycetoma, also known as Madura foot,[1][7] is a type of mycetoma, a persistent fungal infection of the skin and the tissues just under the skin, affecting most commonly the feet, although it can occur in the hands and other body parts.[6] It starts as a painless wet nodule, which may be present for years before ulceration and bone deformity, and results in lumps, grainy discharge and weeping from sinuses.[3][8]
Several fungi can cause eumycetoma,[6] including: Madurella mycetomatis, Madurella grisea, Leptosphaeria senegalensis, Curvularia lunata, Scedosporium apiospermum, Neotestudina rosatii, Acremonium spp. and Fusarium spp..[2] Diagnosis is by visualising the fungi under the microscope and culture of the fluid teased out of the lesion using a sterile needle.[4] If no grains are seen, a biopsy may be required.[4] Medical imaging may reveal extent of bone involvement.[4] Other tests include ELISA, immunodiffusion, and PCR with DNA sequencing.[5] Clinical features are similar to Actinomycetic mycetoma, the bacterial form of mycetoma.[3]
Treatment includes surgical removal of affected tissue and antifungal medicines.[3] The medicine used is guided by the organism cidentified.[4] Itraconazole at a dose of 400 mg daily by mouth may be given for up to year where the cause is Scedosporium apiospermum or the grains are black.[5] Posaconazole at a dose of 400 mg twice daily, is another option.[5] Voriconazole or posaconazole can be used for infections caused by Fusarium spp..[5] After treatment, recurrence is common.[6]
The disease is more common in males aged 20-40 years who work as labourers, farmers and herders.[5] It generally occurs in the tropics,[7] and is endemic in Africa, India and South America.[3] In 2016, the World Health Organization recognised eumycetoma as a neglected tropical disease.[8]
Signs and symptoms
The initial lesion is a small swelling under the skin following minor trauma.[9][10] It appears as a painless wet nodule, which may be present for years before ulceration and bone deformity, and results in a swelling and weeping from sinuses.[3][8] The sinuses discharge a grainy liquid which are fungal colonies.[9] These grains are usually black or white.[11] Destruction of deeper tissues, and deformity and loss of function in the affected limbs may occur in later stages.[12] It tends to occur in one foot.[11] Mycetoma due to bacteria has similar clinical features.[13]
-
Mycetoma, causal organism not specified
-
Mycetoma, causal organism not specified
-
Madura foot
Causes
Eumycetoma is a type of mycetoma caused by fungi. Mycetoma caused by bacteria from the phylum Actinomycetes is different.[9][10] Both have similar clinical features.[13] Fungi causing eumycetoma include: Madurella mycetomatis, Madurella grisea, Leptosphaeria senegalensis, Curvularia lunata, Scedosporium apiospermum, Neotestudina rosatii, Acremonium spp. and Fusarium spp..[2]
The most common fungi causing white discharge is Pseudallescheria boydii.[11][14] Others include fungi of the genus Pseudallescheria, Acremonium and Fusarium.[11]
Black discharge tends to be caused by genera of Madurella, Pyrenochaeta, Exophiala, Leptosphaeria and Curvularia.[11] The most common species are Madurella mycetomatis[11][15] and Trematospheria grisea (previously called Madurella grisea).[11][16]
Mechanism

The disease is acquired by entry of the fungal spores from the soil through a breach in the skin produced by minor trauma like a thorn prick.[17] The disease then spreads to deeper tissues and also forms sinus tracts leading to skin surface.[10] Mature lesions are characterised by a grainy discharge from these sinuses. These discharges contain fungal colonies and are infective. Spread of infection internally through blood or lymph is uncommon.[citation needed]
Infections that produce a black discharge mainly spread subcutaneously. In the red and yellow varieties deep spread occurs early, infiltrating muscles and bones but sparing nerves and tendons, which are highly resistant to the invasion.[18]
Diagnosis
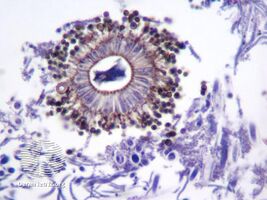
Diagnosis is by biopsy, visualising the fungi under the microscope and culture, which show characteristic fungal filaments and vesicles characteristic of the fungi.[6] Other tests include ELISA, immunodiffusion, and PCR with DNA sequencing.[5]
X rays and ultrasonography may be carried out to assess the extent of the disease. X rays findings are extremely variable. The disease is most often observed at an advanced stage that exhibits extensive destruction of all bones of the foot. Rarely, a single lesion may be seen in the tibia where the picture is identical with chronic osteomyelitis. Cytology of fine needle aspirate or pus from the lesion, and tissue biopsy may be undertaken sometimes.[9] Some publications have claimed a "dot in a circle sign" as a characteristic MRI feature for this condition (this feature has also been described on ultrasound).[12]
-
X-ray foot: mycetoma
-
Aspergillus niger causing eumycetoma
-
Culture: Madurella mycetomatis
Differential diagnosis
Clinical features are similar to Actinomycetic mycetoma, the bacterial form of mycetoma.[3] Botryomycosis, caused by Staphylococcus aureus may produce similar signs and symptoms to eumycetoma.[19]
The following clinical conditions may be considered before diagnosing a patient with mycetoma:[citation needed]
- Tuberculous ulcer
- Kaposi's sarcoma, a vascular tumour of skin usually seen in AIDS.
- Leprosy
- Syphilis
- Malignant neoplasm
- Tropical ulcer[18]
Prevention
No vaccine is available. Simple hygienic precautions like wearing shoes or sandals while working in fields, and washing hands and feet at regular intervals may help prevent the disease.[citation needed]
Treatment
Surgery combined with itraconazole at a dose of 400 mg daily by mouth may be given for up to year where the cause is Scedosporium apiospermum or the grains are black.[5] Posaconazole at a dose of 400 mg twice daily, is another option.[5] Voriconazole or posaconazole can be used for infections caused by Fusarium spp..[5]
Ketoconazole has been used.[20] Actinomycetes usually respond well to medical treatment, but the eumycetes are generally resistant and may require surgical interventions including salvage procedures as bone resection or even the more radical amputation.[21][12][10][12] Amputation may be needed.[17]
Outcome
After treatment, recurrence is common.[6][17]
Epidemiology
The disease is more common in males aged 20-40 years who work as labourers, farmers and herders, and in travellers to tropical regions, where the condition is endemic.[5]
History
Madura foot or maduromycosis or maduramycosis[22] is described in ancient writings of India as Padavalmika, which, translated means Foot anthill.[10] The first modern description of Madura foot was made in 1842 from Madurai (the city after which the disease was named Madura mycosis) in India, by Gill.[10] The fungal cause of the disease was established in 1860 by Carter.[10]
Society and culture
In 2016, the World Health Organization recognised eumycetoma as a neglected tropical disease.[8] Traditionally occurring in regions where resources are scarce, medicines may be expensive and diagnosis is frequently made late, when more invasive treatment may be required.[8] In Sudan in 2015, the cost of treating eumycetoma with itraconazole was around US$26 per day.[8]
References
- ↑ 1.0 1.1 Kutzner, Heinz; Kempf, Werner; Feit, Josef; Sangueza, Omar (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. p. 77-108. ISBN 978-1-119-64706-5. Archived from the original on 2021-06-10. Retrieved 2021-06-07.
- ↑ 2.0 2.1 2.2 2.3 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Archived from the original on 1 August 2018. Retrieved 9 June 2021.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 457. ISBN 978-0-7020-6830-0. Archived from the original on 2021-05-25. Retrieved 2021-06-13.
- ↑ 4.0 4.1 4.2 4.3 4.4 Morris-Jones, Rachael (2019). "18. Tropical dermatology". In Morris-Jones, Rachael (ed.). ABC of Dermatology (7th ed.). Hoboken: Wiley Blackwell. pp. 151–152. ISBN 978-1-119-48899-6. Archived from the original on 2022-05-16. Retrieved 2022-05-17.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Queiroz-Telles, Flavio; Fahal, Ahmed Hassan; Falci, Diego R.; Caceres, Diego H.; Chiller, Tom; Pasqualotto, Alessandro C. (November 2017). "Neglected endemic mycoses". The Lancet. Infectious Diseases. 17 (11): e367–e377. doi:10.1016/S1473-3099(17)30306-7. ISSN 1474-4457. PMID 28774696. Archived from the original on 2021-08-27. Retrieved 2021-08-30.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Estrada, Roberto; Chávez-López, Guadalupe; Estrada-Chávez, Guadalupe; López-Martínez, Rubén; Welsh, Oliverio (July 2012). "Eumycetoma". Clinics in Dermatology. 30 (4): 389–396. doi:10.1016/j.clindermatol.2011.09.009. ISSN 1879-1131. PMID 22682186. Archived from the original on 2021-06-13. Retrieved 2021-06-13.
- ↑ 7.0 7.1 Barlow, Gavin; Irving, Irving; moss, Peter J. (2020). "20. Infectious diseases". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 561. ISBN 978-0-7020-7870-5. Archived from the original on 2021-06-13. Retrieved 2021-06-13.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Emery, Darcy; Denning, David W. (2020). "The global distribution of actinomycetoma and eumycetoma". PLOS Neglected Tropical Diseases. 14 (9): e0008397. doi:10.1371/journal.pntd.0008397. ISSN 1935-2735. PMID 32970667. Archived from the original on 2021-06-13. Retrieved 2022-03-04.
- ↑ 9.0 9.1 9.2 9.3 Davidson's principles and practice of medicine (20th ed.). Churchill Livingstone Elsevier. 2006. p. 373. ISBN 9780443101335.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 Ananthanarayan BA, Jayaram CK, Paniker MD (2006). Textbook of Microbiology (7th ed.). Orient Longman Private Ltd. p. 618. ISBN 978-8125028086.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Bravo, Francisco G. (2020). "14. Fungal, viral and rickettsial infections". In Hoang, Mai P.; Selim, Maria Angelica (eds.). Hospital-Based Dermatopathology: An Illustrated Diagnostic Guide. Switzerland: Springer. pp. 638–664. ISBN 978-3-030-35819-8. Archived from the original on 2021-06-11. Retrieved 2021-06-11.
- ↑ 12.0 12.1 12.2 12.3 El-Sobky, TA; Haleem, JF; Samir, S (2015). "Eumycetoma Osteomyelitis of the Calcaneus in a Child: A Radiologic-Pathologic Correlation following Total Calcanectomy". Case Reports in Pathology. 2015: 129020. doi:10.1155/2015/129020. PMC 4592886. PMID 26483983.
- ↑ 13.0 13.1 "Mycetoma | DermNet NZ". dermnetnz.org. Archived from the original on 13 June 2021. Retrieved 11 June 2021.
- ↑ "Filamentous Fungi". Archived from the original on 2012-08-01. Retrieved 2021-05-25.
- ↑ Ahmed AO, Desplaces N, Leonard P, et al. (December 2003). "Molecular detection and identification of agents of eumycetoma: detailed report of two cases". J. Clin. Microbiol. 41 (12): 5813–6. doi:10.1128/JCM.41.12.5813-5816.2003. PMC 309011. PMID 14662990.
- ↑ Vilela R, Duarte OM, Rosa CA, et al. (November 2004). "A case of eumycetoma due to Madurella grisea in northern Brazil" (PDF). Mycopathologia. 158 (4): 415–8. doi:10.1007/s11046-004-2844-y. PMID 15630550. S2CID 35337823.[permanent dead link]
- ↑ 17.0 17.1 17.2 Zijlstra, Eduard E.; Sande, Wendy W. J. van de; Welsh, Oliverio; Mahgoub, El Sheikh; Goodfellow, Michael; Fahal, Ahmed H. (1 January 2016). "Mycetoma: a unique neglected tropical disease". The Lancet Infectious Diseases. 16 (1): 100–112. doi:10.1016/S1473-3099(15)00359-X. ISSN 1473-3099. Archived from the original on 7 July 2020. Retrieved 14 June 2021.
- ↑ 18.0 18.1 Hamilton Bailey's Demonstrations of Physical Signs in Clinical Surgery ISBN 0-7506-0625-8
- ↑ Devi, B; Behera, B; Dash, ML; Puhan, MR; Pattnaik, SS; Patro, S (2013). "Botryomycosis". Indian Journal of Dermatology. 58 (5): 406. doi:10.4103/0019-5154.117322. ISSN 0019-5154. PMID 24082199. Archived from the original on 2021-08-28. Retrieved 2021-06-14.
- ↑ Capoor MR, Khanna G, Nair D, et al. (April 2007). "Eumycetoma pedis due to Exophiala jeanselmei". Indian J Med Microbiol. 25 (2): 155–7. doi:10.4103/0255-0857.32726. PMID 17582190.
- ↑ Efared, B; Tahiri, L; Boubacar, MS; Atsam-Ebang, G; Hammas, N; Hinde, EF; Chbani, L (2017). "Mycetoma in a non-endemic area: a diagnostic challenge". BMC Clinical Pathology. 17: 1. doi:10.1186/s12907-017-0040-5. PMC 5288886. PMID 28167862.
- ↑ "Infectious Disorders (Specific Agent) Madura foot/Mycetoma/Maduramycosis". MedTech USA, Inc. Archived from the original on 2014-03-22. Retrieved 2013-08-01.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- All articles with dead external links
- Articles with dead external links from March 2022
- Articles with invalid date parameter in template
- Articles with permanently dead external links
- All articles with unsourced statements
- Articles with unsourced statements from July 2020
- Articles with unsourced statements from June 2021
- Articles with unsourced statements from May 2021
- Neglected tropical diseases
- Tropical diseases
- Mycosis-related cutaneous conditions