Eosinophilic cellulitis
| Eosinophilic cellulitis | |
|---|---|
| Other names: Wells' syndrome, recurrent granulomatous dermatitis with eosinophilia[1] | |
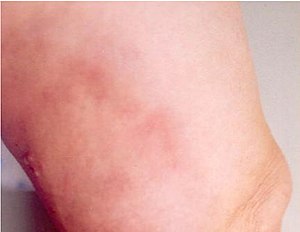 | |
| Initial rash in eosinophilic cellulitis | |
| Specialty | Dermatology |
| Symptoms | Painful, red, raised, warm patches of skin[2] |
| Usual onset | Sudden and recurrent[2] |
| Duration | Few weeks[2] |
| Causes | Unknown[2] |
| Differential diagnosis | Vasculitis, cellulitis, anaphylaxis[2][1] |
| Medication | Corticosteroids, antihistamines[2][1] |
| Prognosis | Often goes away by itself[2] |
| Frequency | ~200 documented cases[1] |
Eosinophilic cellulitis, also known as Wells' syndrome (not to be confused with Weil's disease), is a skin disease that presents with painful, red, raised, and warm patches of skin.[2] The rash comes on suddenly, lasts for a few weeks, and often repeatedly comes back.[2] Scar formation does not typically occur.[1]
Eosinophilic cellulitis is of unknown cause.[2] It is suspected to be an autoimmune disorder.[2] It may be triggered by bites from insects such as spiders, fleas, or ticks, or from medications or surgery.[2] Diagnosis is made after other potential cases are ruled out.[1] Skin biopsy of the affected areas may show an increased number of eosinophils.[2] Other conditions that may appear similar include cellulitis, contact dermatitis, and severe allergic reactions such as anaphylaxis.[2]
Treatment is often with a corticosteroids.[2] Steroids applied as a cream is generally recommended over the use of steroids by mouth.[3] Antihistamines may be used to help with itchiness.[1] Many times the condition goes away after a few weeks without treatment.[2] The condition is uncommon.[1] It affects both sexes with the same frequency.[2] It was first described by George Crichton Wells in 1971.[4][1]
Signs and symptoms
The presentation of this condition consist of edema, cellulitis, and blistering of the skin[5]
-
Wells syndrome
-
Wells syndrome
-
Wells syndrome
Cause
Eosinophilic cellulitis is of unknown cause.[2] It is suspected to be an autoimmune disorder.[2] It may be triggered by bites from insects such as mosquitos,[6] spiders, fleas, or ticks, or from medications or surgery.[2]
Diagnosis
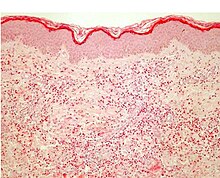
Diagnosis requires ruling out other potential causes.[1] This includes ruling out vasculitis on skin biopsy.[1]
Treatment
Treatment is often with a steroids.[2] This can be either applied as a cream or taken by mouth.[3] As the condition tends to get better on its own taking steroids by mouth should generally only be tried if the rash covers a large area and it does not get better with other measures.[3]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Weins, AB; Biedermann, T; Weiss, T; Weiss, JM (October 2016). "Wells syndrome". Journal der Deutschen Dermatologischen Gesellschaft. 14 (10): 989–993. doi:10.1111/ddg.13132. PMID 27767278.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 "Familial Eosinophilic Cellulitis - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). 2009. Archived from the original on 4 March 2016. Retrieved 10 April 2017.
- ↑ 3.0 3.1 3.2 Räßler, F; Lukács, J; Elsner, P (September 2016). "Treatment of eosinophilic cellulitis (Wells syndrome) - a systematic review". Journal of the European Academy of Dermatology and Venereology : JEADV. 30 (9): 1465–79. doi:10.1111/jdv.13706. PMID 27357601.
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ↑ "Wells syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 18 March 2021. Retrieved 15 May 2021.
- ↑ Tatsuno K, Fujiyama T, Matsuoka H, Shimauchi T, Ito T, Tokura Y (June 2016). "Clinical categories of exaggerated skin reactions to mosquito bites and their pathophysiology". Journal of Dermatological Science. 82 (3): 145–52. doi:10.1016/j.jdermsci.2016.04.010. PMID 27177994.
External links
| Classification |
|---|
- DermNet NZ Archived 2015-08-22 at the Wayback Machine entry


